During the COVID-19 pandemic, we are still seeing MAC patients at UT Health North Campus Tyler. In compliance with current federal guidelines and recommendations, we are encouraging these visits to be conducted via telecommunication when at all possible.
For further information regarding new patient consultations, call 903-877-2899. Current patients will receive a phone call from the nurse one to two days prior to their scheduled appointment to coordinate your visit.
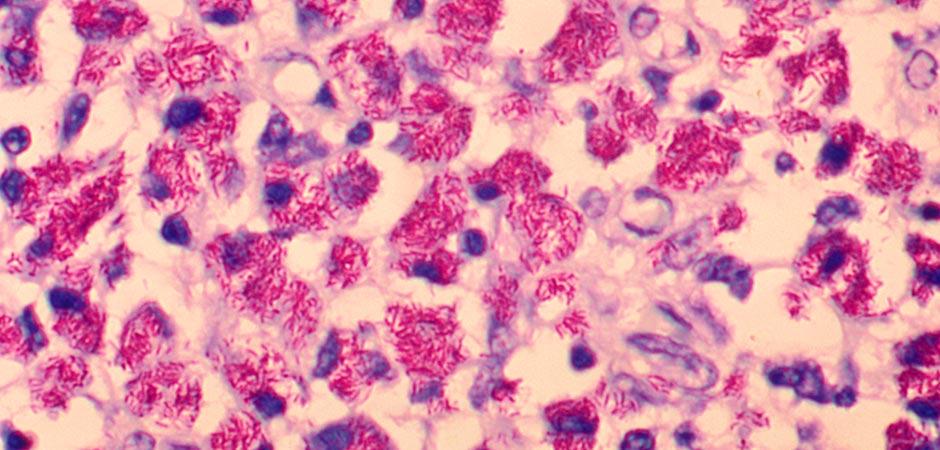
What is Mycobacterium avium complex lung disease (MAC)?
Mycobacterium avium complex (MAC) is an infection caused by a group of bacteria. Mycobacterium avium complex (MAC) is the most common form of nontuberculous mycobacteria (NTM). MAC accounts for more than 80% of all NTM lung disease cases in the U.S.
Symptoms of mycobacterium avium complex lung disease (MAC)
- Cough – You may or may not cough out sputum. NTM lung disease may cause you to cough up blood (this is called hemoptysis). If you cough up blood, you should contact your doctor or seek emergency help immediately. Any time you cough up blood, it is essential that you remain calm and still to help minimize the amount of blood you cough.
- Loss of weight – It is not uncommon to lose weight, which is why it is important to be aware of weight changes. Please consult with your doctor and/or a nutritionist to determine how to modify and augment your diet. You can also find a nutrition guide with suggestions for increasing caloric intake, as well as a printable food diary at ntminfo.org.
- Night sweats – The sensation of feverishness and sweating is often more prominent at night.
- Fatigue
- Chronic cough
- Shortness of breath
Treatment for mycobacterium avium complex lung disease (MAC)
If you are diagnosed with MAC lung disease, you will work with your doctor to make decisions about your treatment options. Because MAC can be challenging to get rid of you should consider finding a pulmonologist or infectious disease specialist with experience treating people with NTM lung disease.
Treatment of MAC lung disease varies from person to person. Not everyone who is diagnosed with MAC lung disease needs to begin treatment right away. Some localized infections are very slow-growing and may or may not progress. If that is the case, your doctor might recommend a watchful waiting period before starting treatment. You would then be monitored with regular follow-up exams to catch any change in your condition before it causes further damage to your lungs.
The standard treatment for most MAC infections is a combination of two or more antibiotics taken over many months. The specific drugs you are prescribed will depend on whether or not the organism has developed any antibiotic resistance. The progress of your treatment will be monitored by collecting follow-up sputum samples. Your disease will only be considered cured when your samples show no sign of MAC infection for at least 12 months. This is to help make sure that your disease does not come back.
Managing mycobacterium avium complex lung disease (MAC):
Taking care of your lungs is critically important to your recovery, especially if you also have bronchiectasis, COPD or another chronic lung disease. Some proven-effective recommendations are:
- Airway clearance techniques are used to reduce the mucus buildup in your lungs and airways. This helps prevent new infections, reduce uncontrolled coughing and improve breathing ability. Chest physical therapy, nebulized hypertonic saline, postural drainage, oscillation vests, chest percussion devices and controlled “huff” coughing can all be used to thin, loosen and expel thick mucus.
- Preventing infections through good hygiene and regular immunizations against influenza and pneumonia, both of which can cause severe complications for people living with NTM and other lung diseases.
- Avoiding exposure to smoke and other lung irritants helps to reduce inflammation that can worsen lung disease. If you are a smoker it is especially important that you quit as soon as possible.
- Other healthy behaviors that will help you manage your MAC disease include:
-
- Exercise to build your endurance, strengthen your breathing ability and lift your mood.
- A well-balanced diet to help you maintain a healthy weight and get the nutrients you need to fight your infection.
-
How to become a new patient
Your primary care physician, pulmonologist or infectious disease physician can refer . Please fax the following information to the referrals department at 903-877-8919.
- Results of sputum cultures for AFB (including the first positive AFB and the last two years of cultures for AFB).
- Results of susceptibility tests on positive AFB cultures, if available.
- Results of routine sputum cultures from the past 12 months, if available.
- Clinical or physician notes (or medical records) that describe your drug treatment, results of bronchoscopy or chest CTs.
- Face – sheet – Demographics and Insurance card.
The patient should bring (preferably on a CD) the following documents to their clinic appointment. The most current CT scans of the chest (within the last 6 months) with written interpretive reports.
Questions should be referred to:
Carolynn Peterson
Patient Hospitality Coordinator
Nontuberculous Mycobacteria Disease (NTM) and Bronchiectasis Clinic
Phone: 903-877-2899
Fax: 903-877-8919
Email: carolynn.peterson@uthct.edu