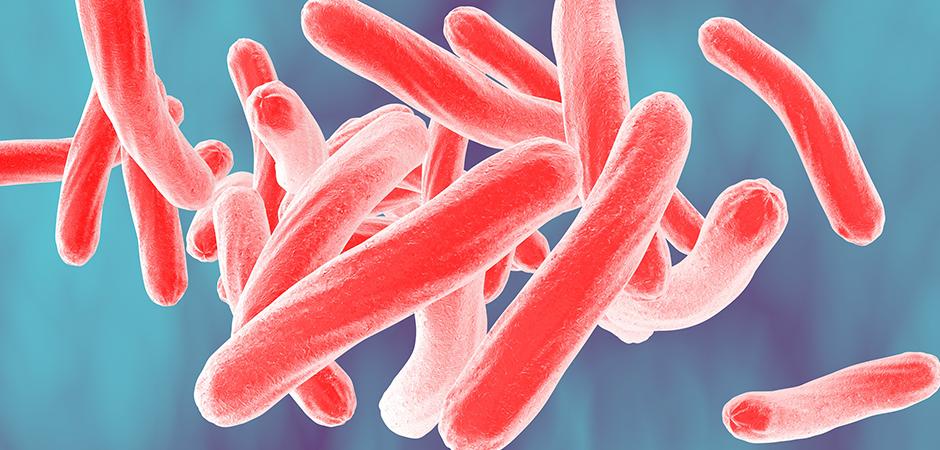
Tuberculosis (TB) is a contagious disease caused by mycobacterium tuberculosis bacteria (Mtb). It is spread through the air when a person with TB coughs, speaks or sings, and people nearby breathe in these bacteria and become infected.
Types of tuberculosis
A TB infection doesn’t always mean that person will get sick. There are two forms of the disease:
- Latent TB - The germs are present in the body, but the immune system keeps them from spreading. The person may not have any symptoms and is not contagious. However, the infection is still alive and can one day become active. If the person is at high risk for re-activation for instance, if they have HIV, have had an infection in the past two years, chest X-ray is unusual or immune system is weakened. They should consult their doctor about medications to prevent active TB.
- Active TB - The germs multiply and make the person sick. The infected person can spread the disease to others. Ninety percent of active cases in adults come from a latent TB infection.
Symptoms of tuberculosis
Symptoms of TB depend on where in the body the TB bacteria are growing. TB bacteria usually grow in the lungs (pulmonary TB). TB disease in the lungs may cause symptoms such as:
- A bad cough that lasts three weeks or longer.
- Pain in the chest.
- Coughing up blood or sputum (phlegm from deep inside the lungs).
Other symptoms of TB disease are:
- Weakness or fatigue.
- Weight loss.
- No appetite.
- Chills.
- Fever.
- Sweating at night.
Symptoms of TB in other parts of the body depend on the area affected. People who have latent TB infection do not feel sick, do not have any symptoms, and cannot spread TB to others.
Treatment for tuberculosis
When TB bacteria become active (multiplying in the body) and the immune system can’t stop the bacteria from growing, this is called TB disease. TB disease will make a person sick. People with TB disease may spread the bacteria to people with whom they spend many hours.
It is very important that people who have TB disease are treated, finish the medicine and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again. If they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat.
TB disease can be treated by taking several drugs for six to nine months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating TB. Of the approved drugs, the first-line anti-TB agents that form the core of treatment regimens are:
- Isoniazid (INH)
- Rifampin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
How is tuberculosis diagnosed?
A skin test and/or a blood test can tell if you have tuberculosis.
For a skin test, you will have a small amount of non-infectious tuberculosis protein injected under the skin of your arm. This protein cannot spread the disease.
It can take two to three days for your skin to react to the injection for a positive result. If it is positive, you will need more tests to find out if you have the latent or active form of tuberculosis. This may include:
- Medical examination
- Chest X-ray
- Testing of some of your phlegm (thick liquid that comes up from your lungs or airways)
Tuberculosis treatment
Tuberculosis can be cured by taking antibiotics. See your healthcare provider for treatment options. It is important for you to take all of your antibiotics as prescribed to avoid spreading pulmonary tuberculosis to others.
To learn more or schedule an appointment for an adult with TB, call:
UT Health East Texas Pulmonary Institute at North Campus Tyler at 903-877-7916
To learn more or schedule an appointment for an pediatric patient with TB, call:
UT Health East Texas Pulmonary Institute at North Campus Tyler at 903-877-5271